4 Questions on NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
5 min read
![]() Dr. Andrea Gruszecki, ND
:
April 23, 2024 at 8:30 AM
Dr. Andrea Gruszecki, ND
:
April 23, 2024 at 8:30 AM

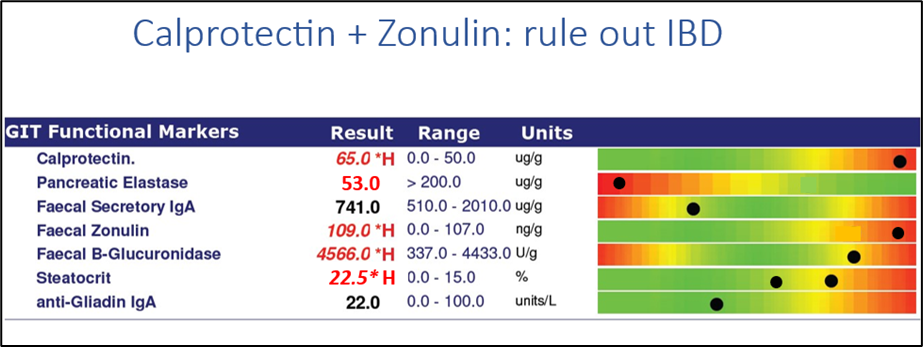
Zonulin, used in conjunction with other fecal inflammation markers such as calprotectin, can help clinicians to distinguish between inflammatory bowel disorders (IBD) and other inflammatory gastrointestinal disorders.
The zonulin biomarker is available on the Advanced GI profile that reflects the level of multiple zonulin family proteins in a blood or stool sample. The zonulin family proteins all share common functions with zonulin and have been clinically associated with increased inflammation in the gut mucosa and elsewhere in the body; for convenience the family of proteins is currently referred to as “zonulin”. Zonulin can be measured in serum or in stool, but since other systemic sources of inflammation (metabolic syndrome, type II diabetes, chronic inflammatory disease, etc.) can raise serum zonulin levels, recent studies indicate that fecal zonulin results may be best when assessing gut function and gut barrier permeability.
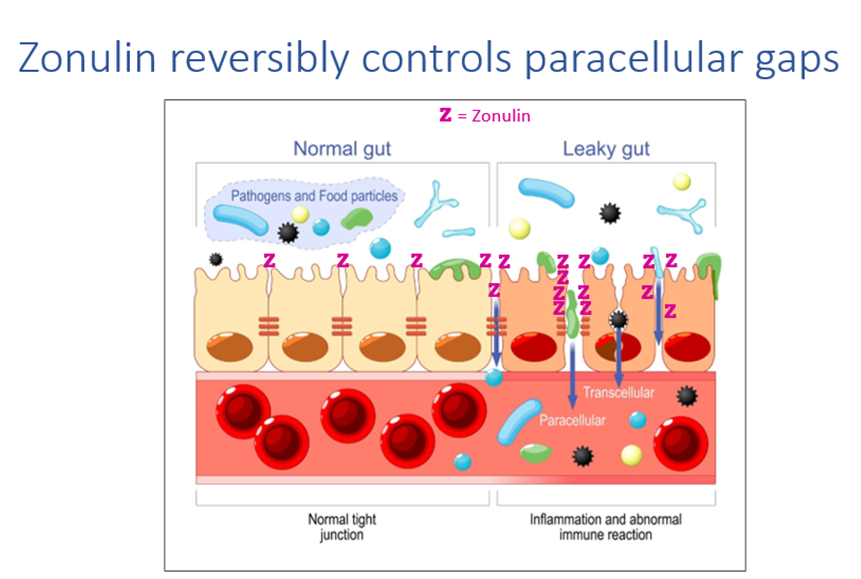
Zonulin family proteins reversibly regulate the paracellular tight junctions that control the gap size between the individual cells that make up the gut mucosal lining. If the paracellular gaps are too wide, foreign proteins can invade the underlying gastrointestinal tissue layers and enter circulation (leaky gut). Circulating foreign proteins increase systemic inflammation and immune system dysregulation. Over time, these foreign proteins can contribute to the induction of environmental allergy and sensitivity. If the foreign substances are mycotoxins, toxic metals or chemicals they can also disrupt immune function and cause inflammation. High levels of both serum and fecal zonulin have been associated with inflammation and increased intestinal permeability, however serum zonulin is less discriminating when assessing gastrointestinal function. Recent human studies indicate that, when combined with other stool markers and knowledge of a patient’s HLA-DQ (Celiac) status that fecal zonulin can be an important diagnostic tool.
Gluten is a protein found in certain grains (wheat, rye, barley) that releases a second protein, called gliadin, during digestion. Gliadin binds to a cellular receptor that promotes the release of zonulin and increases intestinal permeability, stimulating an immune response against gliadin that sets the stage for non-Celiac gluten sensitivity (NCGS) or Celiac disease in HLA-DQ2/8+ individuals. It is likely that genetic variation in the gliadin receptor and along the immune response pathway, in addition to microbiome alterations, digestive status, and other comorbid inflammation, further influence the risk of developing Celiac disease, NCGS, or leaky gut.
Gluten is not the only trigger for intestinal inflammation and increased permeability. Increased intestinal permeability can also occur due to inflammation from:
The inflammatory fecal markers calprotectin, secretory IgA (sIgA), zonulin, -glucuronidase, and anti-gliadin IgA help clinicians to distinguish between autoimmune inflammatory bowel disorders (IBD) and other inflammatory gastrointestinal disorders. Zonulin is useful in the identification of barrier dysfunction in patients with the genetic markers for Celiac disease (HLA-DQ2 and DQ8). Some individuals presenting as non-Celiac gluten-sensitive have Celiac genetics – these individuals, and those with active Celiac disease tend to have elevated fecal zonulin levels. Patients with active inflammatory bowel disease (IBD) also have higher zonulin levels.
Children with both Crohn’s disease and ulcerative colitis have higher fecal zonulin levels than normal controls, while adults with Crohn’s disease tend to have high fecal zonulin levels compared to those with ulcerative colitis or normal controls. Suspect IBD when calprotectin is also elevated. Diarrhea-predominant irritable bowel syndrome (IBS-D) has also been associated with high zonulin levels. However, while most IBS-D patients will have non-diagnostic (lower) calprotectin levels, those with comorbid digestive disorders such as fructose malabsorption, histamine intolerance, lactose intolerance or Helicobacter pylori infection may have an elevated calprotectin level in addition. Patients with Parkinson’s disease have also been shown to have elevated fecal calprotectin and zonulin levels.
It is also important to be aware that the use of immunosuppressive therapies or chemotherapy may prevent the expected elevation of some of the inflammatory and immunology markers on the stool test. Prescription anti-inflammatories, such as steroids or immunosuppressant medications, may depress the level of inflammatory markers on the GI profiles and the medications may also alter the microbiome. As always, a thorough history, review of medication use, and physical examination are just as essential as laboratory findings for correct diagnosis.
Because zonulin reversibly controls paracellular tight junctions it can be used to monitor the restoration of gut barrier function as well as detect barrier dysfunction. Reduction of inflammation and restoration of intestinal permeability may reduce zonulin levels, strengthen the gut barrier and improve gastrointestinal function. Consider:
Zonulin, used in conjunction with other fecal inflammation markers such as calprotectin, secretory IgA (sIgA), -glucuronidase, and anti-gliadin IgA can help clinicians to distinguish between autoimmune inflammatory bowel disorders (IBD) and other inflammatory gastrointestinal disorders. These biomarkers and markers for H. pylori infection and gut microbiome status are all available on US BioTek’s Advanced GI profile; use it today to ensure a complete assessment of your patient’s gastrointestinal health.
References:
Baioumy SA, Elgendy A, Ibrahim SM, Taha SI, Fouad SH. Association between serum zonulin level and severity of house dust mite allergic asthma. Allergy Asthma Clin Immunol. 2021 Aug 31;17(1):86.
Barbaro MR, Cremon C, Morselli-Labate AM, Di Sabatino A, Giuffrida P, et al. Serum zonulin and its diagnostic performance in non-coeliac gluten sensitivity. Gut. 2020 Nov;69(11):1966-1974.
Celebi Sözener Z, Cevhertas L, Nadeau K, Akdis M, Akdis CA. Environmental factors in epithelial barrier dysfunction. J Allergy Clin Immunol. 2020 Jun;145(6):1517-1528.
Del Bo' C, Bernardi S, Cherubini A, Porrini M, Gargari G, Hidalgo-Liberona N, et al. A polyphenol-rich dietary pattern improves intestinal permeability, evaluated as serum zonulin levels, in older subjects: The MaPLE randomised controlled trial. Clin Nutr. 2021 May;40(5):3006-3018.
De Santis S, Cavalcanti E, Mastronardi M, Jirillo E, Chieppa M. Nutritional Keys for Intestinal Barrier Modulation. Front Immunol. 2015 Dec 7;6:612.
El Asmar R, Panigrahi P, Bamford P, Berti I, Not T, Coppa GV, Catassi C, Fasano A. Host-dependent zonulin secretion causes the impairment of the small intestine barrier function after bacterial exposure. Gastroenterology. 2002 Nov;123(5):1607-15.
Fasano A. All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Res. 2020 Jan 31;9:F1000 Faculty Rev-69.
Kapel N, Ouni H, Benahmed NA, Barbot-Trystram L. Fecal Calprotectin for the Diagnosis and Management of Inflammatory Bowel Diseases. Clin Transl Gastroenterol. 2023 Sep 1;14(9):e00617.
Lammers KM, Lu R, Brownley J, Lu B, Gerard C, Thomas K, Rallabhandi P, Shea-Donohue T, Tamiz A, Alkan S, Netzel-Arnett S, Antalis T, Vogel SN, Fasano A. Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology. 2008 Jul;135(1):194-204.e3.
Linsalata M, Riezzo G, Clemente C, D'Attoma B, Russo F. Noninvasive Biomarkers of Gut Barrier Function in Patients Suffering from Diarrhea Predominant-IBS: An Update. Dis Markers. 2020 Oct 13;2020:2886268.
Malíčková K, Francová I, Lukáš M, Kolář M, Králíková E, Bortlík M, Ďuricová D, Štěpánková L, Zvolská K, Pánková A, Zima T. Fecal zonulin is elevated in Crohn's disease and in cigarette smokers. Pract Lab Med. 2017 Sep 23;9:39-44.
Schwiertz A, Spiegel J, Dillmann U, Grundmann D, Bürmann J, Faßbender K, Schäfer KH, Unger MM. Fecal markers of intestinal inflammation and intestinal permeability are elevated in Parkinson's disease. Parkinsonism Relat Disord. 2018 May;50:104-107.
Schnedl WJ, Michaelis S, Enko D, Mangge H. Fecal Calprotectin Elevations Associated with Food Intolerance/Malabsorption Are Significantly Reduced with Targeted Diets. Nutrients. 2023 Feb 27;15(5):1179.
Sciurti M, Fornaroli F, Gaiani F, Bonaguri C, Leandro G, Di Mario F, De' Angelis GL. Genetic susceptibilty and celiac disease: what role do HLA haplotypes play? Acta Biomed. 2018 Dec 17;89(9-S):17-21.
Serek P, Oleksy-Wawrzyniak M. The Effect of Bacterial Infections, Probiotics and Zonulin on Intestinal Barrier Integrity. Int J Mol Sci. 2021 Oct 21;22(21):11359.
Szymanska E, Wierzbicka A, Dadalski M, Kierkus J. Fecal Zonulin as a Noninvasive Biomarker of Intestinal Permeability in Pediatric Patients with Inflammatory Bowel Diseases-Correlation with Disease Activity and Fecal Calprotectin. J Clin Med. 2021 Aug 30;10(17):3905.

Unlocking the Secrets of Cellular Energy
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...