4 Questions on NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
3 min read
![]() Dr. Andrea Gruszecki, ND
:
November 23, 2020 at 9:34 AM
Dr. Andrea Gruszecki, ND
:
November 23, 2020 at 9:34 AM

It seems that almost every attempt to “open up” out of lockdown and get things back to normal is thwarted by a new spike in COVID-19 cases. With the coming holidays, getting accurate information about COVID-19 status for travel purposes or family visits is essential. There have been a great many clinical studies on rapid tests for COVID-19, and the evidence is clear: rapid testing cannot replace laboratory-run RT-PCR assays when screening a symptom-free population that has a low risk of COVID-19 exposure.3
What the study says
A recent study at the University of Arizona found that an emergency-use-authorized (EUA) rapid test used on symptomatic individuals it was in agreement with the gold-standard laboratory real-time PCR (RT-PCR) molecular test about 80% of the time. This means that 20% of positive COVID-19 patients were missed by the rapid test. Other studies have produced similar results.4
The correlation was even lower if the patients screened were free of symptoms or exposure history at the time of testing. In the general population the rapid test could find only 32% of the positive COVID-19 cases identified by the RT-PCR test. This means that rapid tests for COVID-19 are unsuitable for routine travel or work screening.
What’s the problem with rapid tests?
Rapid testing can be useful during spikes or when there are large numbers of infected/symptomatic people in the population; then a positive rapid result may be considered diagnostic.5 Unfortunately, the reverse is not true, and a negative rapid test usually requires a follow-up PCR test. This type of discrepancy is common in viral testing, and this is one reason why many medical centers have a standing policy of performing a laboratory-based PCR test if a symptomatic patient has a negative rapid test result.6 Unfortunately, the need for follow-up testing increases both the cost and the time to diagnosis, which may greatly increase healthcare costs in low-risk populations.
At-home test options do not fare better than rapid tests, as there are significant concerns regarding the sample quality of unsupervised, at-home collections by swabs.7 Even with saliva samples, the Center for Disease Control (CDC) is currently recommending collections under supervision to ensure sample quality.8 Saliva and nasal swabs are both tested using the same RT-PCR methodology, so well-collected samples of either type can reliably detect the COVID-19 virus.9
Why is RT-PCR better?
RT-PCR testing is preferred for COVID-19 virus testing because it is very sensitive and specific for the viral RNA (genetic material). The methodology for Coronavirus RT-PCR testing was during the Severe Acute Respiratory Syndrome (SARS) epidemic of 2002-2003, so that once the genetic code for COVID-19 was determined, highly accurate testing via RT-PCR was quickly available. Rapid tests often use different methodologies that have not been previously evaluated for Coronaviruses. In addition, during shipping the chemical reagents contained within the rapid test cartridges may be subjected to extremes of heat or cold that may affect performance.2 All CAP* and CLIA** certified laboratories are required to perform quality control procedures regularly with positive and negative controls to ensure that tests are performing as expected. The same level of quality control is simply not available for rapid tests.
In conclusion
Recent studies indicate that fever and symptom screening does not reduce COVID-19 transmission.1 For most purposes rapid tests may be considered an adjunct to RT-PCR testing, not a replacement.2 While they may have some utility in emergency medicine, COVID-19 rapid tests are not sufficiently sensitive or specific enough to be used in routine screening for work or travel purposes. US BioTek offers gold-standard PCR testing and provides one of the best turn-around times available for COVID-19 testing. Why not go for the “gold”, and be certain of accurate results?
Learn more about US BioTek's COVID-19 Spike Protein Antibody Tests
* CAP = College of American Pathologists accreditation
** CLIA = Clinical Laboratory Improvement Amendments

Unlocking the Secrets of Cellular Energy
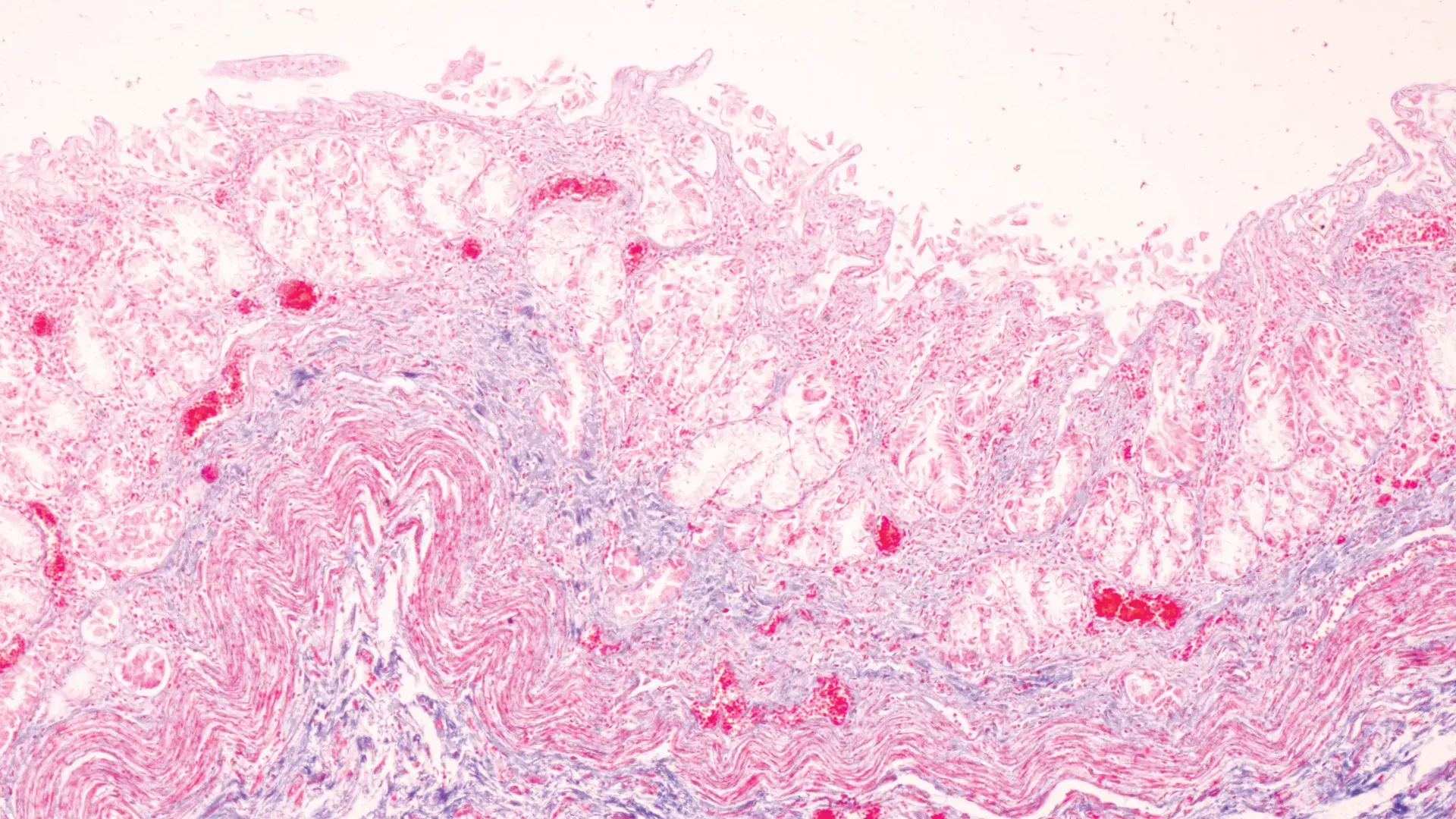
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...