4 Questions on NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
4 min read
![]() Dr. Andrea Gruszecki, ND
:
March 16, 2022 at 5:35 PM
Dr. Andrea Gruszecki, ND
:
March 16, 2022 at 5:35 PM

Oral Allergy Syndrome (OAS), also called pollen-food allergy syndrome (PFAS), is an odd phenomenon. OAS patients present with local IgE-mediated allergic reactions to raw fruits and vegetables. The symptoms of OAS include itchy mouth, scratchy throat, or swelling of the lips, mouth, tongue, and throat. Occasionally, patients will present with itchy ears upon food ingestion instead. The symptoms always begin within minutes of oral contact with the food, and typically subside within an hour.
Oral allergy syndrome is almost always associated with a history of pollen allergy, and it is cross-reactions between proteins in pollens and foods that drive OAS. The problem is that OAS often goes unreported to clinicians because of the transient nature of the symptoms. Unfortunately, OAS can sometimes progress to severe allergic reactions, and even to life-threatening anaphylaxis, over time. Identifying trigger antigens and removing them from the diet and environment may help prevent this progression.
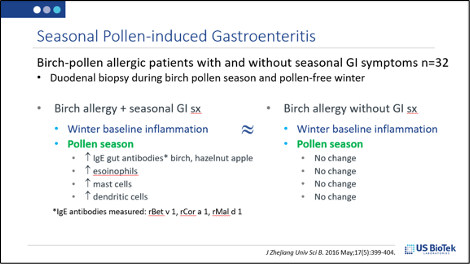
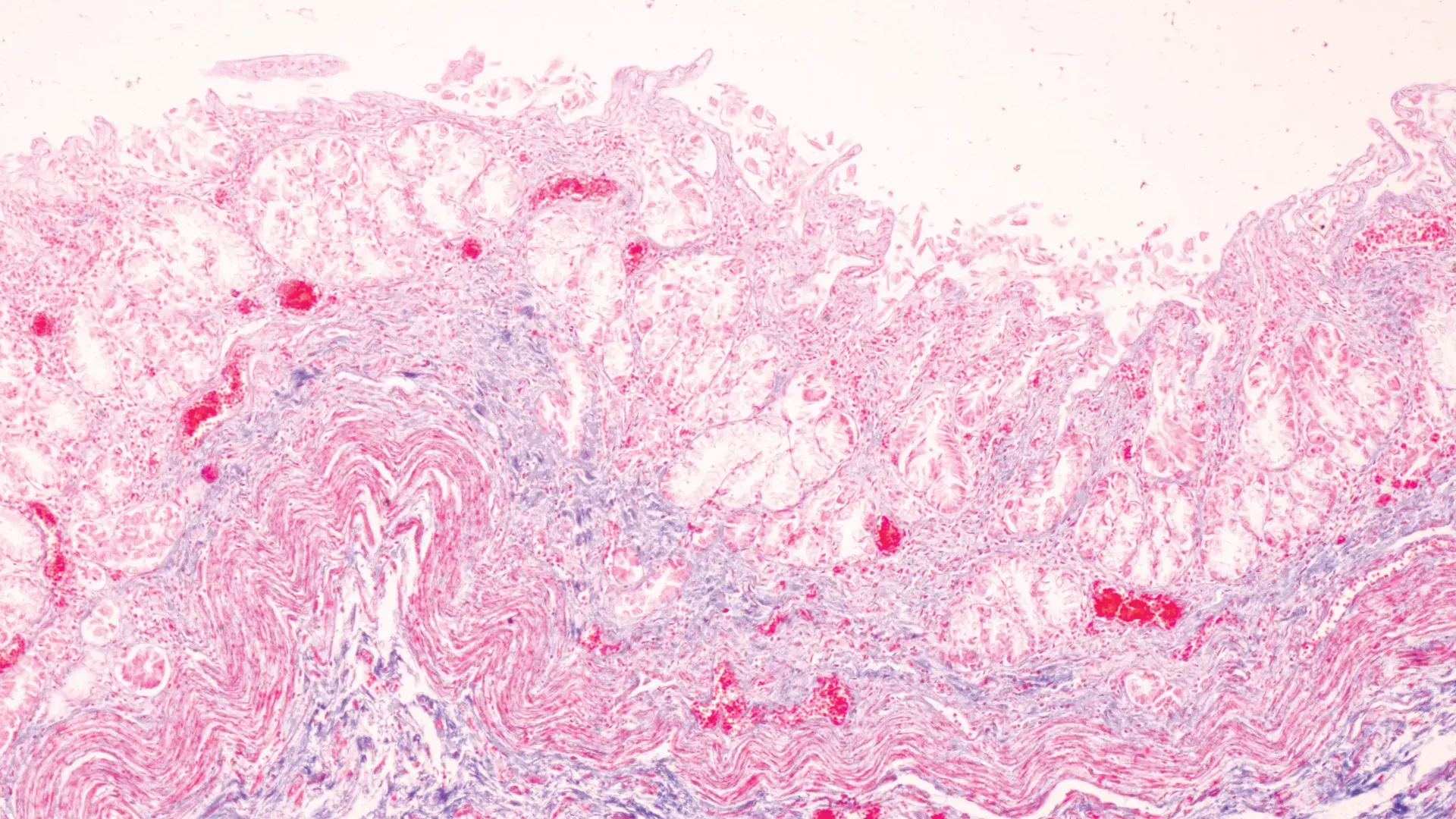
A related reaction can result in pollen-induced gastroenteritis. Neither pollens nor pollen antigens are digested if they are ingested or inhaled and then swallowed. These undigested pollens are immuno-active in the intestinal tract and can induce gut mucosal inflammation in allergic individuals. One study collected duodenal biopsies in pollen season (May-June) and then over local pollen-free months (November-March). As seen below, the birch-allergic patients with gut symptoms had significant changes in their pollen-season biopsy results. Of note, there was an incidental finding; the GI symptomatic patients in this study all had a history of either asthma or OAS.
Human research into IgE allergy syndromes such as OAS frequently include the evaluation of specific IgE component protein (sIgEc). While they are not the only antigenic substances in foods or inhalants, these IgE component proteins are most often the antigens responsible for allergic reactions and atopic disease. sIgEc components associated with increased reactivity risk are bolded in US BioTek’s new IgE Interpretation Guide.
| Peanut | Arachis hypogea | rAra h 9 | nsLTP | Legumes & Nuts |
| Peanut | Arachis hypogea | rAra h 15 | Oleosin | Legumes & Nuts |
| Pecan | Carya illinoensis | Legumes & Nuts | ||
| Pistachio | Pistacia vera | rPis v 1 | 2S Albumin SSP |
Legumes & Nuts |
| Pistachio | Pistacia vera | rPis v 2 | 11S Globulin SSP subunit | Legumes & Nuts |
| Pistachio | Pistacia vera | rPis v 3 | 7/8S Globulin SSP | Legumes & Nuts |
| Soy | Glycine max | rGly m 4 | PR-10 | Legumes & Nuts |
| Soy | Glycine max | rGly m 5 | 7/8S Globulin | Legumes & Nuts |
| Soy | Glycine max | rGly m 6 | 11S Globulin SSP | Legumes & Nuts |
| Soy | Glycine max | rGly m 8 | 2S Albumin SSP | Legumes & Nuts |
sIgEc evaluations can also help determine which cross-reactive foods are the most likely cause of allergic reactions. For example, if a patient is sensitized to silver birch Bet v 1

Look in Table 3 of the Interpretive Guide to see what type of sIgEc that is:
| Silver Birch | Betula verrucosa | rBet v 1 | PR-10 | Tree Pollen |
| Silver Birch | Betula verrucosa | rBet v 2 | Profilin | Tree Pollen |
| Silver Birch | Betula verrucosa | rBet v 6 | Isoflavone Reductase | Tree Pollen |
The bold type indicates that this sIgEc is strongly associated with the risk of allergy and atopic disease. PR-10 is a common sIgEc component, and other plants with profilin antigens, such as timothy grass, are expected to cross-react with Bet v 1. A search of Table 3 indicates that other plants containing PR-10 antigens include alder, beech, hazel, apple, carrot, celery, hazelnut, peanut, peach, soy, and strawberry. We then look to see if the PR-10 antigens in these foods are also reactive, which raises the likelihood that a clinically significant cross-reaction may be causing symptoms. In the example below, apples and strawberries are likely to induce IgE symptoms upon exposure and should be avoided to minimize risk.
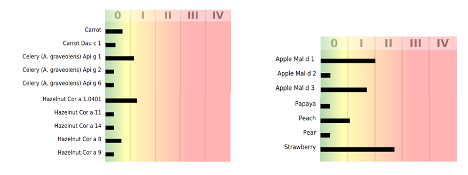
For a patient with allergic symptoms, clinicians may consider eliminating the cross-reactive foods when they reach class I. If the patient is sensitized, we may consider minimizing exposures, and perhaps eliminating during pollen season, foods that reach class II reactivity. Heat treatments (processing or cooking) may change the protein antigen’s structure enough that the patient can tolerate the food cooked, but not raw. However, recent evidence indicates that eating OAS trigger foods cooked may worsen skin conditions such as atopic eczema.
Avoidance of pollen or other cross-reacting inhalant exposures is equally important, and there are measures that patients can take to protect themselves:
In Conclusion:
Manifestations of IgE allergy include OAS, IgE hypersensitivity reactions, IgE-mediated gastroenteritis, and atopic disease. OAS develops after IgE sensitization to pollen pan-allergens occurs. If the patient’s history includes seasonal allergies, consider an IgE-mediated pollen-food cross-reaction in patients with OAS symptoms or seasonal gastrointestinal disorders.
Jagdis A, Kanani A, Stark D. Oral allergy syndrome and risk of food-related anaphylaxis: a cross-sectional survey analysis. All Asth Clin Immun. 2011;7(A2). https://doi.org/10.1186/1710-1492-7-S2-A2
Mastrorilli C, Cardinale F, Giannetti A, Caffarelli C. Pollen-Food Allergy Syndrome: A not so Rare Disease in Childhood. Medicina (Kaunas). 2019 Sep 26;55(10):641.
Osawa Y, Ito Y, Takahashi N, et al. Epidemiological study of oral allergy syndrome in birch pollen dispersal-free regions. Allergology International. 2020 Apr;69(2):246-252.
Rentzos G, Lundberg V, Stotzer PO, Pullerits T, Telemo E. Intestinal allergic inflammation in birch pollen allergic patients in relation to pollen season, IgE sensitization profile and gastrointestinal symptoms. Clin Transl Allergy. 2014;4:19.
Zuidmeer L, van Ree R, Werfel T, Ebner C. Cooking birch pollen-related food: divergent consequences for IgE- and T cell-mediated reactivity in vitro and in vivo. J Allergy Clin Immunol. 2006 Jul;118(1):242-9.

Unlocking the Secrets of Cellular Energy
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...