4 Questions on NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
6 min read
![]() Dr. Andrea Gruszecki, ND
:
August 30, 2023 at 11:22 AM
Dr. Andrea Gruszecki, ND
:
August 30, 2023 at 11:22 AM

Gastrointestinal dysfunction and loss of gut microbiome diversity have been associated with an increased risk of IgE allergy, leaky gut syndrome and sensitivities. Sensitivities are inappropriate immune responses to common environmental antigens such as foods or inhalants. As research into gut-mediated immune responses has progressed, non-IgE-mediated food reactions, or sensitivities, are now acknowledged. These food sensitivity reactions are all mediated, directly or indirectly, by IgA, IgG or IgG-immune complexes and complement activation. The management of IgE allergy is different than for food/inhalant sensitivities and both require a basic understanding of the hypersensitivity responses involved. The symptom profiles for IgE and IgG hypersensitivity are usually easy to distinguish, although some symptoms may overlap.
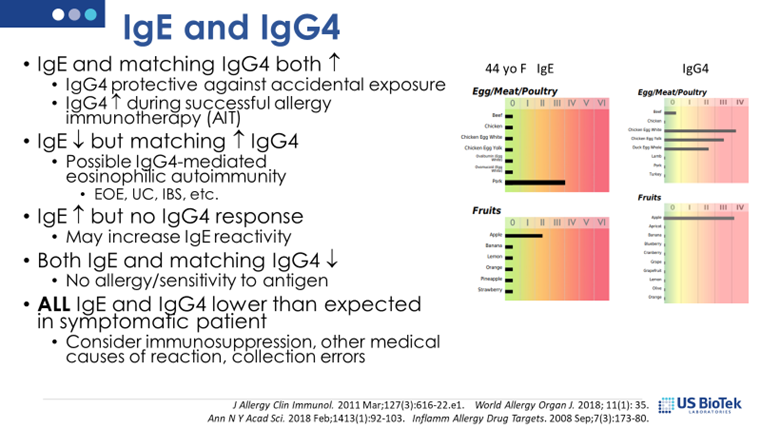
IgE symptoms may present as anaphylaxis (sudden sneezing, coughing or wheezing reaction, difficulty breathing, hives, swelling of lips, tongue, throat, sudden hypotension, sudden GI symptoms) or a less aggressive response; the keynote IgE symptom is consistency. The reaction happens consistently, within minutes to hours, every time food exposure occurs. IgE responses in children may be different, and include symptoms such as rectal bleeding, constipation, colic, dermatitis, chronic nasal congestion, or failure to thrive. IgE allergic responses may be moderated by dose or the presence of IgG4antibodies. IgG4 “competes” with IgE antibodies to block their enzyme activity or protein-protein interactions that cause allergic reactions. IgG4 levels can increase when there is prolonged, chronic exposure to high levels of protein antigens, providing some protection against IgE hypersensitivity. It is important to evaluate both IgE and IgG4 in allergic patients, and it is essential that patients strictly avoid foods that induce allergic reactions.
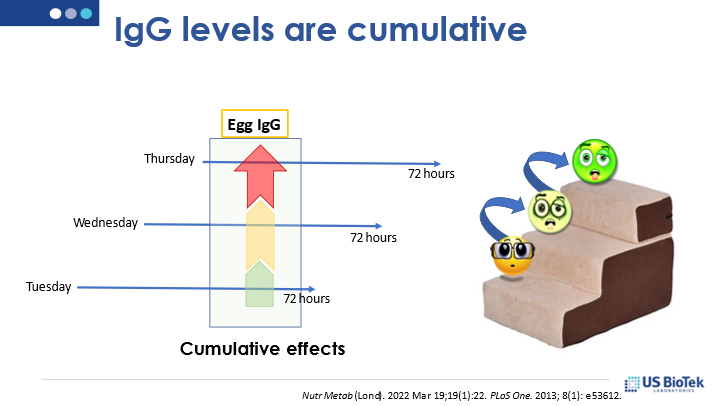
IgG symptoms are different. Symptoms develop over time and may not become apparent until 1-3 days after a food is eaten, or symptoms may be chronic if a food is eaten frequently. IgG sensitivity to foods may contribute to chronic inflammation, either locally or via systemic symptoms such as autoimmune conditions, migraine, skin rashes, asthma, or fatigue, irritability, nervousness, or gastrointestinal symptoms (indigestion, gas, abdominal cramps or bloating). The keynote symptoms here are delayed response and chronicity of symptoms. Food intolerance (sensitivity) may be a symptom of digestive disorders, genetic enzyme deficiencies, gut microbiome imbalances, as well as the result of IgG or other non-IgE mediated immune responses.
Allergy or sensitivity reactions in the gastrointestinal system can result in local inflammation and loss of gut barrier functions. The gut mucosa and the immune system may be further influenced by diet and nutrition, and the gut-associated lymphoid tissue (GALT) system uses essential dietary components (such as lipids and vitamins) as modulatory molecules to maintain the gut mucosa and maintain immune tolerance. Some essential vitamins and compounds, such as B-vitamins and short-chain fatty acids, are produced in the gut by bacteria in the gut microbiome. A loss of diversity in the gut microbiome may result in a shortage of essential nutrients and anti-inflammatory signaling molecules.
Knowledgeable clinicians can employ a series of steps to manage both food sensitivity and inhalant allergies, improve tolerance, and provide patient relief:
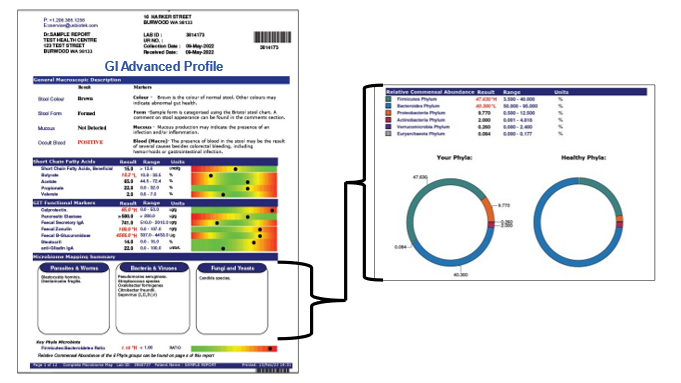
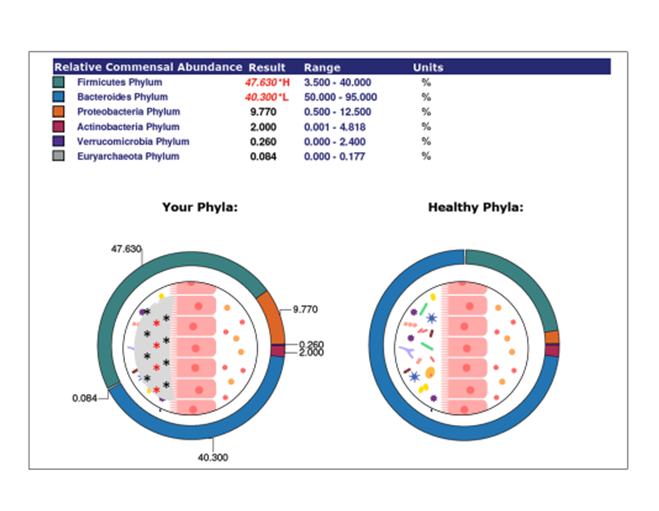
US BioTek’s stool testing may be used to evaluate digestion, absorption, and microbiome diversity. Based upon the results of a GI profile, a clinician may choose to improve diet quality and/or provide nutritional support. Action steps may include:
Gastrointestinal dysfunction and loss of gut microbiome diversity induce proinflammatory changes in the gut mucosal lining and immune reactivity. These changes increase the risk of IgE allergy, IgG or IgA food sensitivity, and compromise gut barrier functions. IgE allergy, IgA and IgG sensitivity and stool testing can provide guidance for therapeutic interventions to restore gut homeostasis and immune tolerance required for health and wellness.
References:
Celebi Sözener Z, Cevhertas L, Nadeau K, Akdis M, Akdis CA. Environmental factors in epithelial barrier dysfunction. J Allergy Clin Immunol. 2020 Jun;145(6):1517-1528.https://pubmed.ncbi.nlm.nih.gov/32507229/
Goldin BR, Swenson L, Dwyer J, Sexton M, Gorbach SL. Effect of diet and Lactobacillus acidophilus supplements on human fecal bacterial enzymes. J Natl Cancer Inst. 1980 Feb;64(2):255-61.https://pubmed.ncbi.nlm.nih.gov/6766508/#:~:text=The%20addition%20of%20viable%20Lactobacillus,beta%2Dglucuronidase%20and%20nitroreductase%20activities.
Haque SZ, Haque M. The ecological community of commensal, symbiotic, and pathogenic gastrointestinal microorganisms - an appraisal. Clin Exp Gastroenterol. 2017 May 5;10:91-103.https://pubmed.ncbi.nlm.nih.gov/28503071/
Kim WJ, Choi IS, Kim CS, Lee JH, Kang HW. Relationship between serum IgA level and allergy/asthma. Korean J Intern Med. 2017 Jan;32(1):137-145. https://pubmed.ncbi.nlm.nih.gov/27586868/
Kim YS, Kim JW, Ha NY, Kim J, Ryu HS. Herbal Therapies in Functional Gastrointestinal Disorders: A Narrative Review and Clinical Implication. Front Psychiatry. 2020 Jul 10;11:601.https://pubmed.ncbi.nlm.nih.gov/32754057/
Łoniewska B, Fraszczyk-Tousty M, Tousty P, Skonieczna-Żydecka K, Maciejewska-Markiewicz D, Łoniewski I. Analysis of Fecal Short-Chain Fatty Acids (SCFAs) in Healthy Children during the First Two Years of Life: An Observational Prospective Cohort Study. Nutrients. 2023 Jan 11;15(2):367.https://pubmed.ncbi.nlm.nih.gov/36678236/
Pan g T, Leach ST, Katz T, Day AS, Ooi CY. Fecal biomarkers of intestinal health and disease in children. Front Pediatr. 2014 Jan 28;2:6.https://pubmed.ncbi.nlm.nih.gov/24479111/
Schwarz A, Panetta V, Cappella A, Hofmaier S, Hatzler L, et al. IgG and IgG4 to 91 allergenic molecules in early childhood by route of exposure and current and future IgE sensitization: Results from the Multicentre Allergy Study birth cohort. J Allergy Clin Immunol. 2016 Nov;138(5):1426-1433.e12. https://pubmed.ncbi.nlm.nih.gov/27264457/
Siddiqui I, Majid H, Abid S. Update on clinical and research application of fecal biomarkers for gastrointestinal diseases. World J Gastrointest Pharmacol Ther. 2017 Feb 6;8(1):39-46. https://pubmed.ncbi.nlm.nih.gov/28217373/
Sobral MMC, Gonçalves T, Martins ZE, Bäuerl C, Cortés-Macías E, Collado MC, Ferreira IMPLVO. Mycotoxin Interactions along the Gastrointestinal Tract: In Vitro Semi-Dynamic Digestion and Static Colonic Fermentation of a Contaminated Meal. Toxins (Basel). 2022 Jan 1;14(1):28. https://pubmed.ncbi.nlm.nih.gov/35051005/
Tian X, Deng Z, Wang S, Wang Y. Basic Research and Clinical Reports Associated with Low Serum IgG4 Concentrations. Int Arch Allergy Immunol. 2020;181(2):149-158. https://pubmed.ncbi.nlm.nih.gov/31805576/
Vidarsson G, Dekkers G, Rispens T. IgG subclasses and allotypes: from structure to effector functions. Front Immunol. 2014 Oct 20;5:520. https://pubmed.ncbi.nlm.nih.gov/25368619/
Vitte J, Vibhushan S, Bratti M, Montero-Hernandez JE, Blank U. Allergy, Anaphylaxis, and Nonallergic Hypersensitivity: IgE, Mast Cells, and Beyond. Med Princ Pract. 2022;31(6):501-515. https://pubmed.ncbi.nlm.nih.gov/36219943/
Yu LC. Intestinal epithelial barrier dysfunction in food hypersensitivity. J Allergy (Cairo). 2012;2012:596081.https://pubmed.ncbi.nlm.nih.gov/21912563/
Zheng R, Zhang Y, Zhang K, Yuan Y, Jia S, Liu J. The Complement System, Aging, and Aging-Related Diseases. Int J Mol Sci. 2022 Aug 4;23(15):8689. https://pubmed.ncbi.nlm.nih.gov/35955822/

Unlocking the Secrets of Cellular Energy
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...