4 Questions on NAD/NADH Testing Answered
Unlocking the Secrets of Cellular Energy
4 min read
![]() Dr. Andrea Gruszecki, ND
:
July 19, 2022 at 8:30 AM
Dr. Andrea Gruszecki, ND
:
July 19, 2022 at 8:30 AM

While the pitter-patter of little feet in the office can be a joy, clinicians must remember that pediatric patients may differ from adult patients in many regards. Differences may include a higher ratio of IgE true allergy, lower infant levels of IgG4, maternal antibody donation and different sample collection strategies. A good history, assessment and sample collection can streamline the evaluation of pediatric patients.
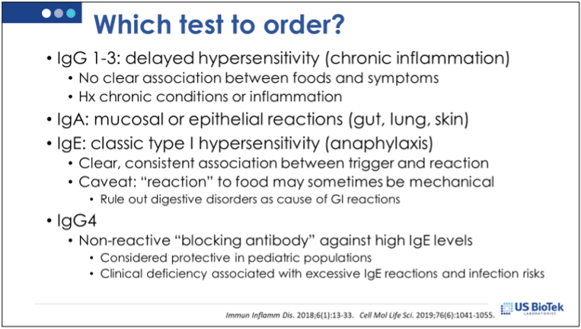
Different types of antibodies provide different types of information. Very high levels of any of the antibody classes can contribute to a patient’s overall inflammation status. IgG1-3 and IgA are associated with delayed inflammatory reactions that can take up to 72 hours to manifest.
IgG classes 1-3 can activate pro-inflammatory complement cascades associated with chronic inflammatory conditions. High levels of IgG 1-3 overload receptors and drive the inflammatory reaction while low levels of IgG indicate tolerance. If only IgG1-3 are high, then often a food can be safely re-introduced after a period of abstinence.
Circulating serum IgA levels are different from secretory IgA (sIgA) measured in the stool. Serum IgA levels have been associated with allergy and asthma, but like IgG1-3, high IgA levels can contribute to delayed hypersensitivity reactions and chronic inflammation. These IgA reactions can indicate foods or inhalants that may be directly irritating to the mucosal lining (gut, lung) or skin.
IgE is associated with immediate hypersensitivity (true allergy). While the rate of IgE allergy diagnosis in adults and pediatric patients is about the same, children may have higher rates of skin atopy and rhinitis than adults and be more susceptible to symptoms from food allergy. Once sensitization has occurred, IgE reactivity can persist for years due to the presence of long-lived B-memory cells. Ideally, IgE and IgG4 are tested together, because IgG4 does not activate complement, but instead is a “blocking antibody” for IgE.
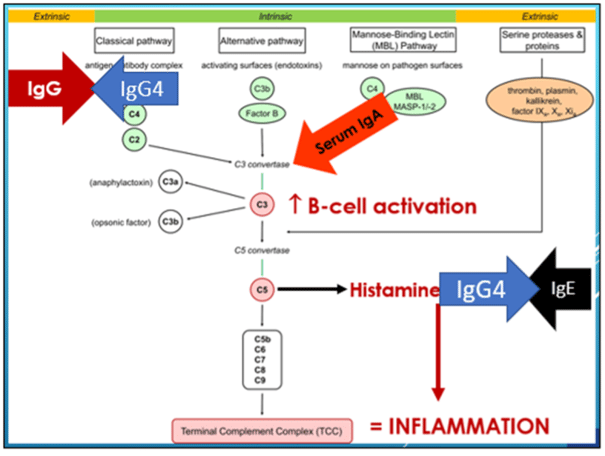
IgG4 levels are typically low in infants, who tend to respond to higher IgE levels with IgG1 elevation. Class-switching from IgG1 to IgG4 appears to coincide with weaning and food introduction in human studies. The presence of IgG4 is protective in children, not inflammatory, as IgG4-IgE binding tends to decrease IgE reactivity. When infants and young children demonstrated increased IgE levels and allergic/atopic symptoms, IgG4 levels were usually closely associated with IgE elevations.
While rare, selective IgG4 class deficiency may occur in up to 15% of the population, and often goes undetected. Since IgG4 deficiency is associated with both increased IgE reactivity and increased risk of infections, and dual IgE/IgG4 assessment in weaned pediatric patients is clinically relevant in symptomatic patients.
Several studies have investigated the induction of IgE, IgG and IgG4 during infancy and childhood, but none have accounted for breast-feeding, weaning and food introduction. This oversight is unfortunate, as circulating maternal antibodies are known to transfer during breast-feeding, and it is possible that lower functional levels of maternal IgG4 may be present in infants until weaning.
When the evaluation of breast-feeding pediatric patients is necessary, the impact of maternal antibodies must be considered by the clinician. Both IgE and IgG antibodies pass from the maternal circulation into the breast milk, although levels in the milk are lower than levels in the blood. Current evidence indicates that certain milk proteins typically found in breast milk do not seem to raise specific antibodies, but all other types of antibodies (including pollen antibodies) may be found in the breast milk and can dictate the nursing infant’s immune responses.
If the patient is primarily breast-fed, then a blood sample from the infant reflects maternal antibody status. In such cases, the mother may be tested instead of the infant, and both mother and infant then avoid the antigens causing allergy or sensitivity. Once the child is weaned, the effect of maternal antibodies will fade within weeks for IgE, and within several months for IgG. Formula-fed infants can be tested directly as the effect of maternal antibodies on test results will fade over weeks to months.
Obtaining blood samples from pediatric patients can be challenging, so getting the right test done with the right type of sample is crucial. While dried bloodspot samples may seem attractive for pediatric patients, these collections may be contraindicated in very young patients. Clinicians need to be aware of the following factors when pediatric antibody testing is required:
When pediatric patients require antibody testing, clinicians can improve their clinical success by reviewing a checklist of considerations specific to children. Pediatric patients may differ from adult patients in many regards including the rate of IgE true allergy in pediatric patients, lower infant levels of IgG4, effects of maternal antibody donation and sample collection strategies. A good history, assessment and sample collection can streamline the evaluation of pediatric patients, and may improve clinical success.
Amos JA. (2017) Allergies Statistics and Facts. Healthline.com. https://www.healthline.com/health/allergies/statistics Reviewed 05 July 2022.
Hochwallner H, Alm J, Lupinek C, Johansson C, Mie A, et al. Transmission of allergen-specific IgG and IgE from maternal blood into breast milk visualized with microarray technology. J Allergy Clin Immunol. 2014;134(5):1213-1215.
Jenmalm MC, Björkstén B. Development of immunoglobulin G subclass antibodies to ovalbumin, birch and cat during the first eight years of life in atopic and non-atopic children. Pediatr Allergy Immunol. 1999 May;10(2):112-21.
Kim JH, Park HJ, Choi GS, Kim JE, Ye YM, Nahm DH, Park HS. Immunoglobulin G subclass deficiency is the major phenotype of primary immunodeficiency in a Korean adult cohort. J Korean Med Sci. 2010 Jun;25(6):824-8.
Nursekey.com (2020) Blood Drawing From Peripheral Sites: Heel Stick and Finger Stick. https://nursekey.com/blood-drawing-from-peripheral-sites-heel-stick-and-finger-stick/ Reviewed 06 July 2022.
Ohsaki A, Venturelli N, Buccigrosso TM, Osganian SK, Lee J, Blumberg RS, Oyoshi MK. Maternal IgG immune complexes induce food allergen-specific tolerance in offspring. J Exp Med. 2018 Jan 2;215(1):91-113.
Schwarz A, Panetta V, Cappella A, Hofmaier S, Hatzler L, et al. IgG and IgG4 to 91 allergenic molecules in early childhood by route of exposure and current and future IgE sensitization: Results from the Multicentre Allergy Study birth cohort. J Allergy Clin Immunol. 2016 Nov;138(5):1426-1433.e12.
Voloshin S, Smoldovskaya O, Feyzkhanova G, Arefieva A, Pavlushkina L, et al. Patterns of sensitization to inhalant and food allergens among pediatric patients from the Moscow region (Russian Federation). PLoS One. 2018 Mar 22;13(3):e0194775.
WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy. Geneva: World Health Organization; 2010. 7, Capillary sampling. https://www.ncbi.nlm.nih.gov/books/NBK138654/#_NBK138654_pubdet_ Reviewed 06 July 2022.

Unlocking the Secrets of Cellular Energy
Short chain fatty acids (SCFAs) are organic acids produced by bacterial fermentation of dietary fibre and resistant starch. Enterocytes and...

Zonulin has emerged as a popular marker to assess the integrity of the intestinal mucosal barrier. Discovered by Dr Alessio Fasano, Zonulin...